Systematic review reveals psilocybin reduces obsessive-compulsive behaviours across clinical and preclinical evidence

From compulsive behaviors to potential therapeutic interventions. (Left) Excessive hand-washing illustrating compulsive behaviors characteristic of obsessive-compulsive disorder. (Right) Psilocybe cubensis mushrooms containing psilocybin.
Landmark synthesis examines 13 studies spanning clinical trials and validated animal models, identifying consistent anti-compulsive effects.
What distinguishes this synthesis from previous reviews is its ambitious scope and rigorous methodology. The research team conducted systematic searches of PubMed using carefully constructed search strings that captured studies examining psilocybin, psilocin, or psilocybin-containing mushrooms in relation to obsessive-compulsive symptoms or behaviours. Their search, conducted in March 2025 with an updated search in September 2025, initially identified 370 articles, which after applying rigorous exclusion criteria yielded 13 studies meeting inclusion standards. The synthesis followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, ensuring transparent and reproducible methodology. What makes this review particularly timely is the growing recognition that psilocybin's therapeutic applications may extend beyond mood disorders to conditions characterized by repetitive, ritualistic behaviours.
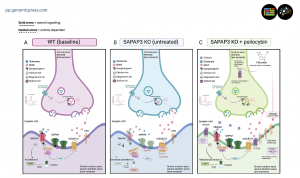
The studies analyzed span diverse methodological approaches, from open-label clinical trials to randomized pharmacological challenges, and from acute behavioural assessments in wild-type rodents to longitudinal studies in genetic knockout models. The clinical studies involved patients with treatment-resistant obsessive-compulsive disorder and body dysmorphic disorder, conditions that share core features of distressing intrusive thoughts and repetitive behaviours. Preclinical investigations employed multiple behavioural paradigms, including marble-burying tests in wild-type mice and excessive grooming assessments in SAPAP3 knockout mice, which lack a postsynaptic protein crucial for striatal function and display compulsive behaviours analogous to human obsessive-compulsive disorder. This breadth of evidence, spanning species and methodologies, strengthens confidence in the patterns identified through synthesis.
But what does the clinical evidence actually reveal about psilocybin's therapeutic potential? The clinical trials synthesized demonstrate consistent reductions in obsessive-compulsive symptoms following psilocybin administration. In the earliest study examined, conducted by Moreno and colleagues in 2006, nine patients with treatment-resistant obsessive-compulsive disorder received escalating doses of psilocybin ranging from 25 to 300 micrograms per kilogram orally. Marked decreases in symptom severity, measured by the Yale-Brown Obsessive-Compulsive Scale, were observed in all participants during one or more sessions, with reductions ranging from 23 to 100 percent. The effects manifested between four and 24 hours after ingestion, demonstrating rapid onset. Intriguingly, the therapeutic response showed no significant dose-dependent relationship, suggesting that lower doses may retain efficacy.
More recent investigations have expanded the evidence base to related conditions within the obsessive-compulsive spectrum. Schneier and colleagues in 2024 examined psilocybin's effects in 12 adults with body dysmorphic disorder who had not responded adequately to serotonin reuptake inhibitor treatment. A single 25-milligram oral dose produced significant reductions in symptom severity at one, two, three, six, and 12 weeks following administration, with large effect sizes persisting throughout the follow-up period. At the 12-week endpoint, seven participants met response criteria, with four also achieving remission. Body dysmorphic disorder shares neurobiological features with obsessive-compulsive disorder and is classified within the same diagnostic cluster. This finding suggests psilocybin's therapeutic potential extends across the obsessive-compulsive and related disorders spectrum.
A retrospective online survey by Buot and colleagues in 2023 gathered data from 135 participants who had consumed psilocybin-containing mushrooms and met criteria for obsessive-compulsive disorder. Participants reported significant improvements in obsessive-compulsive symptomatology following psilocybin use, with approximately 30 percent of users reporting persistent benefits lasting more than three months. Individuals who consumed psilocybin-containing mushrooms on multiple occasions reported stronger symptom improvements than single-use individuals, suggesting potential for repeated dosing strategies.
Beyond acute clinical responses, how do psilocybin's effects manifest in controlled laboratory models? The preclinical evidence synthesized reveals a crucial distinction between transient effects in wild-type rodents and sustained therapeutic responses in validated disease models. In wild-type mice, psilocybin acutely decreased marble-burying behaviour, a commonly used measure of compulsive-like digging. Studies by Matsushima, Odland, and Singh demonstrated that psilocybin administration 15 to 30 minutes before testing reduced the number of marbles buried. However, these effects were time-limited and did not persist beyond the first day after administration.
The marble-burying test has faced criticism regarding its validity as a model of compulsive behaviour, as the digging response in wild-type mice may reflect exploratory behaviour rather than pathological compulsion. This interpretive challenge underscores the importance of employing validated genetic models that more faithfully recapitulate the neurobiological underpinnings of obsessive-compulsive disorder.
Where does the most compelling preclinical evidence emerge? The most compelling preclinical evidence comes from studies using SAPAP3 knockout mice, which lack the SAPAP3 postsynaptic scaffolding protein highly expressed in the striatum. These mice display excessive grooming behaviour that, if untreated, causes skin lesions, mimicking the compulsive, harmful repetitive behaviours seen in obsessive-compulsive disorder. The human ortholog of this gene has been implicated in patients with obsessive-compulsive disorder and pathological grooming, and the mice exhibit corticostriatal circuit dysfunction that parallels abnormalities observed in human patients.
Multiple studies demonstrate that psilocybin produces sustained reductions in excessive grooming in SAPAP3 knockout mice. Investigations by Estrada and colleagues revealed that a single psilocybin injection reduced excessive grooming for up to one week after administration, with effects manifesting within hours and persisting throughout the observation period. Subsequent research by Thompson extended these findings, showing that psilocybin at doses of one and two milligrams per kilogram reduced excessive grooming when assessed one, seven, 14, and 21 days after administration, with effects maintaining statistical significance through three weeks post-injection.
These persistent behavioural changes in a validated disease model contrast sharply with the transient effects observed in wild-type animals, suggesting that psilocybin's anti-compulsive actions require pathological neural substrates to manifest fully. The durability of therapeutic effects following single administration represents a clinically significant feature distinguishing psilocybin from conventional pharmacotherapies that require continuous dosing to maintain efficacy.
What neurobiological mechanisms might explain these remarkable sustained effects? The sustained nature of psilocybin's effects in SAPAP3 knockout mice implicates neuroplastic mechanisms rather than acute receptor occupancy. Conventional serotonergic treatments for obsessive-compulsive disorder require weeks of continuous administration before therapeutic effects emerge and symptoms typically return rapidly following treatment discontinuation. In contrast, psilocybin produces effects within hours that persist for weeks after single administration, suggesting fundamental alterations in neural circuitry rather than transient neurochemical changes.
Studies examining molecular correlates of psilocybin's effects in SAPAP3 knockout mice provide mechanistic clues. Thompson and colleagues found that psilocybin increased cortical expression of markers associated with synaptic plasticity, including brain-derived neurotrophic factor and components of the mammalian target of rapamycin signaling pathway. These molecular changes temporally correlated with behavioural improvements and persisted beyond the period of acute drug effects, consistent with a neuroplasticity-mediated mechanism.
The leading hypothesis proposes that psilocybin, through 5-HT2A receptor activation, triggers cascades of molecular events that promote dendritic remodeling, synaptogenesis, and circuit reorganization. In disease states characterized by maladaptive circuit function, such as the corticostriatal abnormalities in obsessive-compulsive disorder, these neuroplastic changes may facilitate the emergence of more adaptive neural patterns, effectively "resetting" pathological circuits.
An underappreciated strength of this synthesis lies in its expansion beyond narrowly defined obsessive-compulsive disorder to the full spectrum of related conditions. The demonstration that psilocybin reduces symptoms in body dysmorphic disorder, coupled with preclinical evidence that it diminishes compulsive behaviours in genetic models, suggests transdiagnostic therapeutic potential across conditions sharing core features of repetitive, ritualistic behaviours and distorted cognitions.
Building on these findings, the review authors propose a comprehensive research agenda for the next decade. Highest priority involves conducting adequately powered, randomized, placebo-controlled trials with active placebo controls and functional neuroimaging to assess whether psilocybin normalizes the frontostriatal hyperactivity characteristic of obsessive-compulsive disorder. Dosing strategy comparisons represent another research priority—determining whether clinicians should aim for single high doses, repeated moderate doses, or chronic microdosing regimens. At the preclinical level, mechanistic investigations should employ validated genetic models to dissect the molecular and cellular pathways mediating sustained anti-compulsive effects.
Dr. Thibault Renoir, the corresponding author and senior investigator on this review, holds a Ronald Philip Griffiths Fellowship from the University of Melbourne. Prof. Anthony Hannan, a senior author, holds a Principal Research Fellowship from the National Health and Medical Research Council and leads a laboratory investigating gene-environment interactions in neurological and psychiatric conditions. The team at the Florey Institute of Neuroscience and Mental Health brings together expertise in behavioural neuroscience, psychopharmacology, and translational psychiatry.
This systematic review represents a critical synthesis of current knowledge on psilocybin's effects across the obsessive-compulsive and related disorders spectrum, providing researchers, clinicians, and policymakers with a comprehensive framework for understanding both established findings and critical gaps. By systematically analyzing and integrating findings from 13 studies spanning clinical trials in treatment-resistant populations and validated animal models, the authors reveal patterns invisible in individual studies, particularly the consistency of anti-compulsive effects across diverse methodological approaches. The rigorous methodology employed, including systematic database searches following PRISMA guidelines and transparent inclusion criteria, ensures the reliability and reproducibility of the synthesis, exemplifying how systematic analysis of existing literature can generate new understanding and guide research resources toward the most critical unanswered questions.
The Review in Psychedelics titled "Psilocybin's effects on obsessive-compulsive behaviours: A systematic review of preclinical and clinical evidence," is freely available via Open Access on 28 October 2025 in Psychedelics at the following hyperlink: https://doi.org/10.61373/pp025i.0044.
An accompanying editorial, titled "From compulsive behaviors to psychedelic therapeutics: When mice and man speak the same circuit language," is published in the same issue of Psychedelics on 28 October 2025. The editorial contextualizes the systematic review's findings within the broader landscape of psychedelic research, examining the translational significance of cross-laboratory replication in animal models and discussing future research directions needed to advance psilocybin-based treatments for obsessive-compulsive and related disorders. The editorial is freely available via Open Access at: https://doi.org/10.61373/pp025d.0047.
About Psychedelics: Psychedelics: The Journal of Psychedelic and Psychoactive Drug Research (ISSN: 2997-2671, online and 2997-268X, print) is a peer reviewed medical research journal published by Genomic Press, New York. Psychedelics is dedicated to advancing knowledge across the full spectrum of consciousness altering substances, from classical psychedelics to stimulants, cannabinoids, entactogens, dissociatives, plant derived compounds, and novel compounds including drug discovery approaches. Our multidisciplinary approach encompasses molecular mechanisms, therapeutic applications, neuroscientific discoveries, and sociocultural analyses. We welcome diverse methodologies and perspectives from fundamental pharmacology and clinical studies to psychological investigations and societal-historical contexts that enhance our understanding of how these substances interact with human biology, psychology, and society.
Visit the Genomic Press Virtual Library: https://issues.genomicpress.com/bookcase/gtvov/
Our full website is at: https://genomicpress.com/
For technical information on this work, please contact Dr. Thibault Renoir at the Florey Institute of Neuroscience and Mental Health, Melbourne Brain Centre, University of Melbourne, Parkville, VIC 3052, Australia. E-mail: thibault.renoir@unimelb.edu.au.
Ma-Li Wong
Genomic Press
mali.wong@genomicpress.com
Visit us on social media:
LinkedIn
Bluesky
Instagram
Facebook
X
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.